CLINICAL AUDITS
CLINICAL AUDIT EXAMINING THE RESPONSE SENT TO PATIENTS WITH AN INTENTIONAL OVERDOSE BY THE LAS
7 pages
The clinical audit shows that almost half of the patients triaged at the time of the call as intentional overdose, but with no life threatening symptoms, had to wait for more than 30 minutes for a response. Most crews spent less than an hour on scene with the patient. However, due to the length of time patients waited for a response, the LAS was still responsible for the care of two thirds of patients over an hour after the initial 999 call.
Queries regarding this clinical audit … Telephone the Clinical Audit & Research Unit - 0207 783 2504.
7 pages
The clinical audit shows that almost half of the patients triaged at the time of the call as intentional overdose, but with no life threatening symptoms, had to wait for more than 30 minutes for a response. Most crews spent less than an hour on scene with the patient. However, due to the length of time patients waited for a response, the LAS was still responsible for the care of two thirds of patients over an hour after the initial 999 call.
Queries regarding this clinical audit … Telephone the Clinical Audit & Research Unit - 0207 783 2504.
|
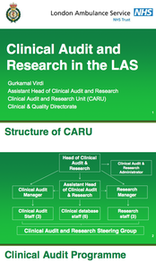
CLINICAL AUDIT AND RESEARCH IN THE LAS
18 pages Examples of recent projects
|
A CLINICAL AUDIT EXAMINING 'END OF LIFE CARE' IN THE LONDON AMBULANCE SERVICE
February 2012 - 22 pages
Clinical Audit Reports examining end of life care provided to patients by the LAS and documentation of end tidal CO2 for patients with advanced airway adjuncts.
The end of life care Clinical Audit aimed to assess the knowledge and confidence crews have regarding patients who are at the end stage of a terminal illness, and the care provided to this patient group. Findings show that very few patients had an out-of-hours form registered on the LAS database, as a result the majority of patients were taken to A&E. When the patient was not attended to at the request of a healthcare professional, some crews consulted with the patients’ GP or a member of their palliative care team. Most crews considered whether the patient was experiencing pain and discomfort, with subsequent action being taken for the majority patients. The patients’ wishes were not documented for most patients but the patients’ diagnosis and prognosis was clearly documented for nearly every patient. Referrals were also felt to be appropriate for most patients. More than half the members of staff who responded to the questionnaire stated they had ‘very low’ or ‘some confidence’ in treating end stage of a terminally ill patients. When asked to explain low levels of confidence, respondents said they felt they needed more training.
The end-tidal CO2 (ETCO2) baseline Clinical Audit was conducted to assess documentation of ETCO2 and if waveforms are being used to inform the care given to patients where an advanced airway adjunct is used. At least one ETCO2 reading was documented for the majority of patients. ETCO2 readings were documented more frequently in crews second set of observations than in their initial set of observations. Very few waveforms were submitted as part of the clinical record. Where an ETCO2 reading was documented, this reading was not zero for any patients. Therefore, it was not necessary for the ambulance crew to retry the placement of the airway adjunct.
February 2012 - 22 pages
Clinical Audit Reports examining end of life care provided to patients by the LAS and documentation of end tidal CO2 for patients with advanced airway adjuncts.
The end of life care Clinical Audit aimed to assess the knowledge and confidence crews have regarding patients who are at the end stage of a terminal illness, and the care provided to this patient group. Findings show that very few patients had an out-of-hours form registered on the LAS database, as a result the majority of patients were taken to A&E. When the patient was not attended to at the request of a healthcare professional, some crews consulted with the patients’ GP or a member of their palliative care team. Most crews considered whether the patient was experiencing pain and discomfort, with subsequent action being taken for the majority patients. The patients’ wishes were not documented for most patients but the patients’ diagnosis and prognosis was clearly documented for nearly every patient. Referrals were also felt to be appropriate for most patients. More than half the members of staff who responded to the questionnaire stated they had ‘very low’ or ‘some confidence’ in treating end stage of a terminally ill patients. When asked to explain low levels of confidence, respondents said they felt they needed more training.
The end-tidal CO2 (ETCO2) baseline Clinical Audit was conducted to assess documentation of ETCO2 and if waveforms are being used to inform the care given to patients where an advanced airway adjunct is used. At least one ETCO2 reading was documented for the majority of patients. ETCO2 readings were documented more frequently in crews second set of observations than in their initial set of observations. Very few waveforms were submitted as part of the clinical record. Where an ETCO2 reading was documented, this reading was not zero for any patients. Therefore, it was not necessary for the ambulance crew to retry the placement of the airway adjunct.
A BASELINE CLINICAL AUDIT EXAMINING THE MEASUREMENT OF ETCO2 DURING ADVANCED AIRWAY MANAGEMENT OF CARDIAC ARREST PATIENTS BY THE LONDON AMBULANCE SERVICE
February 2011 - 5 pages
When a patient experiences a cardiac arrest, it is important that a patient’s airway is secured as this will enable the practitioner caring for the patient to perform continuous chest compressions, without the need to pause for ventilation (JRCALC, 2006). An airway should be secured using an advanced airway adjunct; these adjuncts include endotracheal tubes (ET) and supraglottic airway devices (SGA), such as a Laryngeal Mask Airway and i-Gel.
February 2011 - 5 pages
When a patient experiences a cardiac arrest, it is important that a patient’s airway is secured as this will enable the practitioner caring for the patient to perform continuous chest compressions, without the need to pause for ventilation (JRCALC, 2006). An airway should be secured using an advanced airway adjunct; these adjuncts include endotracheal tubes (ET) and supraglottic airway devices (SGA), such as a Laryngeal Mask Airway and i-Gel.